For many, adjusting to dentures is more than a routine change—it’s a shift that comes with challenges, some more surprising than others. One issue that often flies under the radar is denture stomatitis, a common yet frequently underestimated condition that can lead to redness, irritation, and even infection beneath the dentures. It’s uncomfortable, it’s persistent, and for some patients, it becomes a recurring frustration that affects their quality of life. At Atkins Dental Clinic, we’ve seen how traditional dentures—while helpful in restoring basic function—can contribute to these issues.
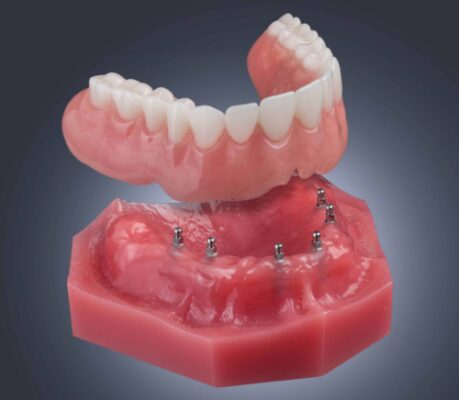
Implant dentures offer a more stable, healthier alternative. By anchoring the denture to the jawbone with mini dental implants, we eliminate the slipping and rubbing that often lead to inflammation. The result is a more secure fit, fewer pressure points, and a dramatically reduced risk of tissue irritation. If you’re tired of fighting with your dentures and ready for a more reliable solution, we’re here to help you take that next step.
Defining Denture Stomatitis
Denture stomatitis is an oral condition that develops beneath dentures, especially on the roof of the mouth. It involves inflammation of the tissue in direct contact with the denture surface. This inflammation appears as redness, swelling, and in some cases, pinpoint areas of bleeding. Even though it may sound alarming, denture stomatitis often progresses without pain, which can delay detection.
The main trigger behind this condition is an overgrowth of Candida albicans—a yeast organism naturally present in the mouth. Dentures, by design, create an enclosed space between the acrylic base and the soft tissue. That warm, moist, and shaded environment allows yeast to multiply far more easily than in exposed areas of the mouth.
While Candida plays a central role, several other factors can pave the way for this condition. Inadequate denture hygiene leaves behind food particles and bacteria that contribute to irritation. Wearing dentures continuously, without removing them overnight, prevents tissues from recovering and increases the likelihood of infection. Poorly fitting dentures can add mechanical stress and friction, further compromising the health of the tissue.
Certain systemic conditions and medications also increase the risk. People with diabetes, for example, face a higher chance of developing oral infections, including denture stomatitis. Medications that reduce saliva flow create a dry oral environment—another factor that encourages yeast overgrowth.
Symptoms can vary widely. Some individuals experience soreness, a burning sensation, or an unpleasant taste in the mouth. Others notice dryness, persistent bad breath, or patches of redness and white lesions on the tissue under the denture. In some cases, cracks or sores may form at the corners of the lips. Because the appearance of the affected area often mirrors the shape of the denture, clinicians can usually identify the condition by sight.
How To Prevent Denture Stomatitis
Part One: Denture Hygiene
Treating denture stomatitis begins with restoring balance in the mouth—and that means putting daily care at the forefront. The goal is to reduce inflammation, control yeast overgrowth, and give the oral tissues time to heal.
Hygiene plays a leading role. Dentures should be cleaned every day with mild soap or a non-abrasive denture cleanser. Regular toothpaste can damage the denture’s surface, so it’s best avoided. After meals, rinsing the denture under running water helps eliminate trapped food particles that can contribute to bacterial buildup.
At night, soaking the denture in a cleaning solution or plain water keeps the material from drying out and warping. This step is especially important because dentures need to remain moist to maintain their fit and function.
Oral tissues deserve attention, too. Brushing the gums, tongue, and roof of the mouth with a soft toothbrush stimulates circulation and helps clear away lingering bacteria. Rinsing with an alcohol-free mouthwash or warm saltwater solution offers extra support for healing and hygiene.
Just as important as cleaning is rest. Dentures should be removed for at least six to eight hours a day—typically overnight—to allow the gums to recover from the pressure of daily wear. Giving the mouth this downtime is one of the most effective ways to reduce irritation.
Part Two: A Smarter Approach to Denture Fit
Even the most meticulous hygiene routine can fall short if the denture itself no longer fits properly. Over time, the shape of the jawbone changes—especially when teeth are missing. That’s because traditional dentures, while replacing the visible parts of teeth, don’t replace the roots. Without tooth roots to stimulate the jawbone, the bone begins to shrink in a process known as resorption.
As this happens, dentures that once fit snugly can start to slip, shift, and irritate the gums. Adhesives may help for a while, but they don’t address the underlying issue: the absence of a stable foundation.
Dental implants provide a long-term solution by restoring that foundation. Dr. Aaron places these small titanium posts into the jawbone, where they function as artificial tooth roots. They stimulate the bone, prevent further resorption, and offer a secure anchor for dentures. Whether in the form of implant-retained (removable) or implant-supported (non-removable) options, these solutions provide superior stability, reduce tissue irritation, and dramatically lower the risk of recurring denture stomatitis.
Ready To Feel Comfortable in Your Dentures Again?
If denture stomatitis has been a quiet but persistent presence in your daily life, it’s time to consider what better support could look like. At Atkins Dental Clinic, we understand the frustration of recurring irritation and the limitations of traditional dentures.
With modern implant solutions, you don’t have to settle for discomfort or constant adjustments. A more secure, more stable fit is within reach—and so is renewed confidence in your smile. Contact us today to schedule a free consultation!